For much of their history European cities have been unhealthy places. Until the end of the nineteenth century, they were traversed by waves of infection that would thrive in the close assemblage of people and livestock. Urban mortality rates were so great that sustained migration from the countryside was the only way cities could maintain their population levels stable.1
This may seem a distant past now that “health” is understood in opposition either to aging or to diseases, such as cancer, that are non-communicable. Yet, not only do infectious diseases remain a major cause of death outside Western countries, but scientists agree that the number of epidemic events around the world has actually been increasing. Zika and Ebola are only two prominent examples of “emerging infectious diseases” (EID), a definition that was put forward in the 1990s by American virologist Stephen S. Morse.2 It is also widely accepted within biomedical science that there is a strong nexus between EIDs and the material footprint of capitalist processes of extraction and accumulation: mining, logging, and intensive agriculture have the effect of fragmenting wild habitats, increasing the risk of human exposure to pathogens in the wildlife.3
In spite of such evidence, infectious diseases are conspicuously absent from the architectural discourse on urbanization. This arguably stems from a narrow understanding of the “urban,” which is still limited to the scale of the Western city. As Rem Koolhaas and others have argued, our focus on urban cores has made us blind to the human-driven changes that are taking place outside of them—whether in the countryside or in tropical rainforests.
Among the epidemics that are new to the twentieth century, HIV is by far the deadliest. Discovered in 1983, its cumulative death toll currently exceeds thirty million people and shows little sign of abating.4 The history of its appearance—when and how it first became a human virus—exposes the root of the contemporary entanglement between pathogens, humans, and the environment.
Modernity and Health
Contrary to non-communicable diseases, epidemics are a direct function of urbanization: viruses, bacteria, and parasites can propagate only where enough people live close to one another. If a person catches a virus but dies before having a chance to transmit it to someone else, no epidemic will take place. The size, density, and distribution of human settlements are thus crucial in determining how an epidemic spreads. This is why epidemics can only develop in settled societies—nomadic or seminomadic communities are generally too small and far apart for pathogens to spread effectively. Recent evidence indicates that it was only after the onset of agriculture and of animal husbandry—around 10,000 years ago—that epidemics became a regular presence in human history.5
There is a close correspondence between the history of infectious diseases and the history of the modern city. The first pandemic that may be considered “modern” was the bubonic plague, which regularly visited European cities from the fourteenth until the late-eighteenth century. The catastrophic impact of the plague threatened to destroy the social order of cities, setting in motion a political response in the form of quarantine and isolation wards—the earliest public health protocols.6
In the nineteenth century, industrialization and globalization were paralleled by the onset of cholera and the intensification of tuberculosis. As Michel Foucault noted, these new diseases led to a corresponding shift in the modes of epidemic control—from the exclusion of infected bodies to the management of risk in the population as a whole.7 The fear of cholera in Europe and North America led to the reorganization of the city as a means of controlling individual health. Sanitary reforms first made their way on the political agenda in the 1840s and 1850s with the founding of local health authorities and the construction of new urban systems, such as sewerage, public parks, and “hygienic” expansions based on gridded plans. Yet the laissez-faire capitalism that prevailed at the time favored the persistence of old medical paradigms (such as the miasma theory), delaying coordinated action by several decades. Cholera epidemics continued, and it was only in the 1890s—with the discovery of bacteria and viruses—that public health became a matter of state intervention, and centralized planning a political necessity. The provision of clean drinking water and of subsidized housing were then recognized as universal goals, as were new medical protocols of immunization and disinfection.8 The concern with hygiene transformed urban planning long before it influenced architecture; only at the turn of the twentieth century did architects begin to internalize sanitary prescriptions. By the 1920s, whiteness, air, and light had all become central tenets in the work of Le Corbusier, Alvar Aalto, Walter Gropius, and many other pioneers of the Modern movement. Modernism was founded on the promise of hygienic, urban, and social order.9
By the time the World Health Organization was founded in 1948, the worst infectious diseases (like malaria, smallpox, and cholera) were disappearing from Western Europe and North America, with most others being brought under control by vaccination. Medicine turned its attention to non-communicable pathologies, and the emphasis shifted from collective hygiene to personal health. Epidemics came to be represented as remote occurrences and were naturalized as one of the attributes of the so-called Third World. Yet, the discovery of HIV as the cause of AIDS in 1983 challenged such optimistic narratives.
When the virus first appeared, an incomplete understanding of its biology favored—as is often the case with epidemics—the stigmatization and criminalization of the behavior of individuals and entire communities.10 In particular, the high occurrence of AIDS in sub-Saharan Africa contributed to the continued othering of the African subject and of an entire continent. Together with Ebola, AIDS reinforced Western representations of the African tropics as a hotbed of disease—an epistemological construct that dates back to the early colonial period.11
Yet recent advances in microbiology have cast a different light on the history of infectious diseases, making it possible to analyze the spatial and political contexts that lie behind their emergence. We now know that “pathogens” can live for millennia in other animal species or in water with no apparent effect, and only become disease agents when entering into contact with and adapting to humans. This means that epidemics are less a natural phenomenon than a result of human intervention in the environment. A significant example is cholera, which did not exist until the East India Company encouraged the colonization of the Bengali wetlands in the eighteenth century. It was the exposure of the settler population to the Vibrio cholerae bacterium, which lives in the region’s brackish waters, that led to the first epidemic outbreak in 1817.12
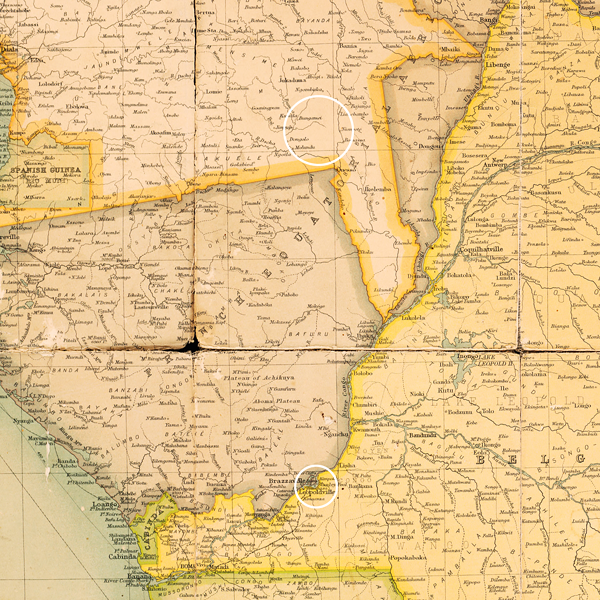

Detail from a 1910 map of central Africa showing the region where HIV-1 is thought to have been transmitted from chimpanzees (upper circle) and the location of Léopoldville (lower circle). The Atlantic railway is visible as a thin black line connecting Léopoldville to the mouth of the Congo river. Source: Stanford University/University of Cape Town Libraries.
Viruses and Genes
Where and how HIV started infecting humans is a question that has preoccupied scientists ever since its discovery. A crucial contribution has come from the refinement of phylogenetic analysis, a technique that makes it possible to reconstruct the evolution of an organism by comparing different samples of its genome. Since a virus like HIV is continuously evolving in order to survive, the chronology of mutations visible in its DNA can reveal a great deal about its history. A turning point in HIV research came in 2008, with the fortuitous discovery of a forgotten sample of human tissue in Kinshasa. The sample, dating from 1960, was found to contain traces of HIV-1.13 A group of scientists guided by Michael Worobey, an evolutionary biologist, compared its DNA to the only other known “pre-historic” sample of HIV (which is from 1959 and was also retrieved in Kinshasa). The scientists found the genetic difference between the two samples so large that it suggested the existence of a “common ancestor” as early as the 1920s—thus disproving the idea of HIV as a recent pathology. They also observed that “the rise of cities may have facilitated the initial establishment and the early spread of HIV-1,” compounding earlier hypotheses that pointed at Kinshasa as the epidemic’s epicenter.14 At the same time as Worobey’s work, another team of scientists guided by virologist Beatrice Hahn determined that HIV-1 is the evolution of SIV, a virus of the common chimpanzee (Pan troglodytes troglodytes). They also were able to pin down, through extensive fieldwork among wild chimpanzee colonies, the area where the first human infection took place: the rainforests of southeastern Cameroon, north of the town of Ouesso.15
These and other discoveries have confirmed that AIDS did not “begin” in the 1980s but considerably earlier. Its story can be reconstructed as follows. SIV was transmitted from chimpanzees to humans between 1900 and 1915. After the first successful infection in the forest, the virus reached Kinshasa in the early 1920s, which was at the time the growing capital of the Belgian Congo. Finding a dense population of human hosts, the virus diversified as HIV-1 and started spreading undetected, and later expanded to other Congolese cities along colonial transportation routes. After the Belgian Congo became independent in 1960, HIV was transported across the Atlantic by Haitians functionaries sent by the UN to replace Belgian ones, leading to the current pandemic.16
Such scientific evidence draws colonial geographies into the picture. With the unprecedented expansion of Europe around the globe, two new major pandemics—cholera and HIV—began at the sites of sudden and intense exploitation of tropical environments—the Bengal under the East India Company, and equatorial Africa under French and Belgian rule.
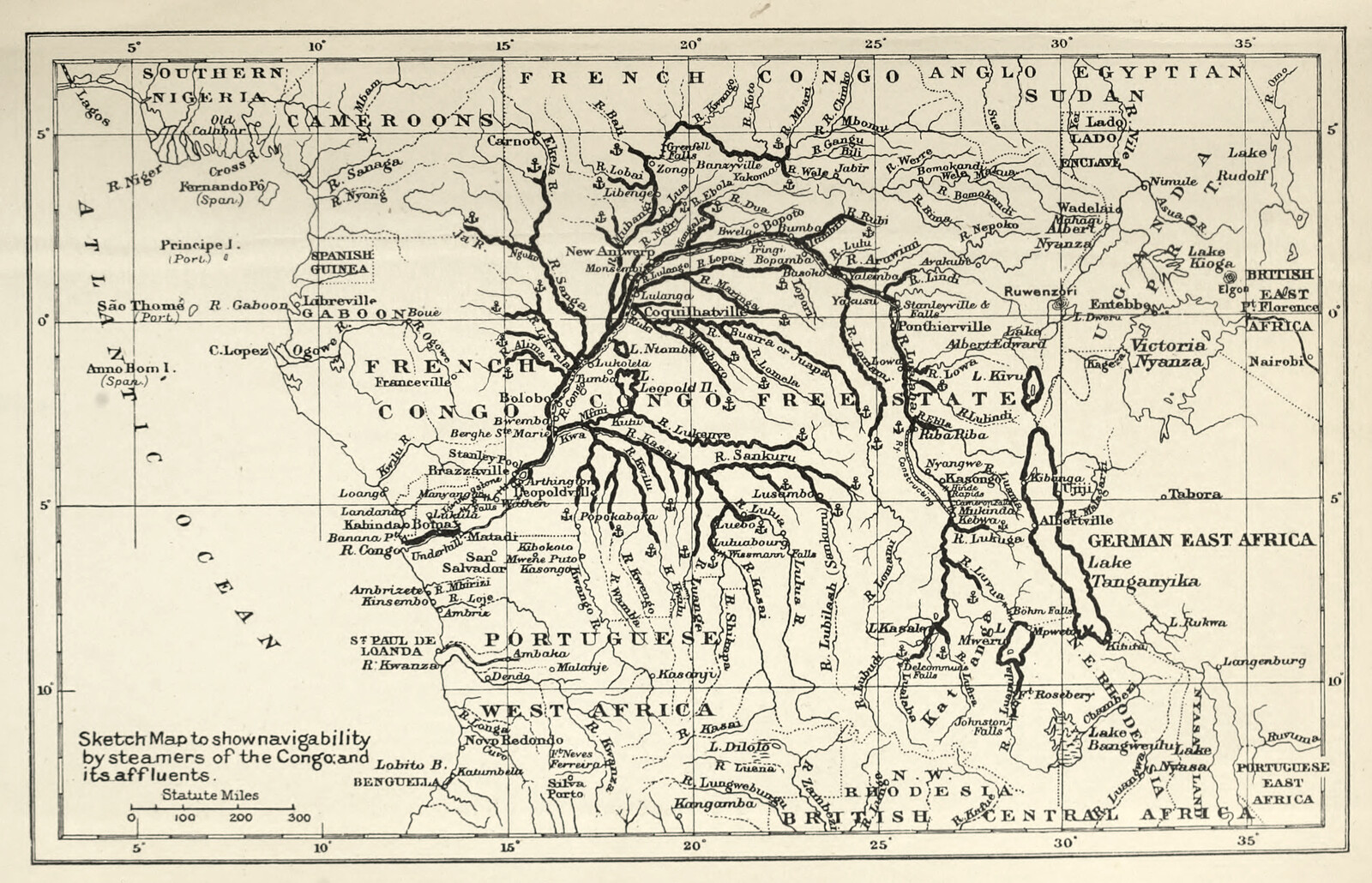
The Congo river as a transportation infrastructure. Source: Harry Johnston, George Grenfell and the Congo, vol. I (London, 1908), 495.
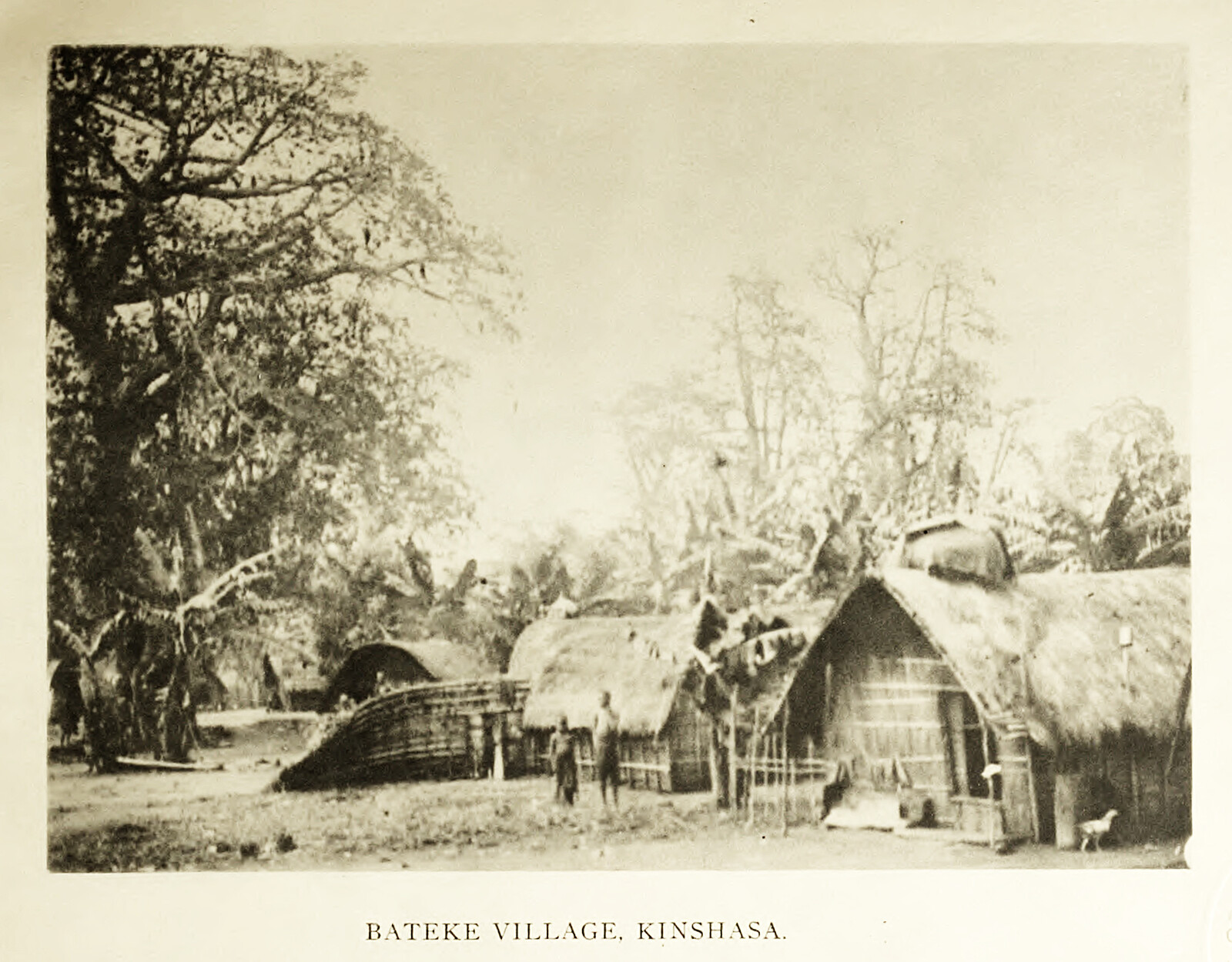
Precolonial village near the site of the city of Kinshasa. The photograph was taken in 1905 by Manuel Gonzales who traveled with Frederick Starr, an American colonial anthropologist as well as an apologist for King Leopold. Source: Frederick Starr, Congo Natives: An Etnographic Album (Chicago, 1912), plate III.
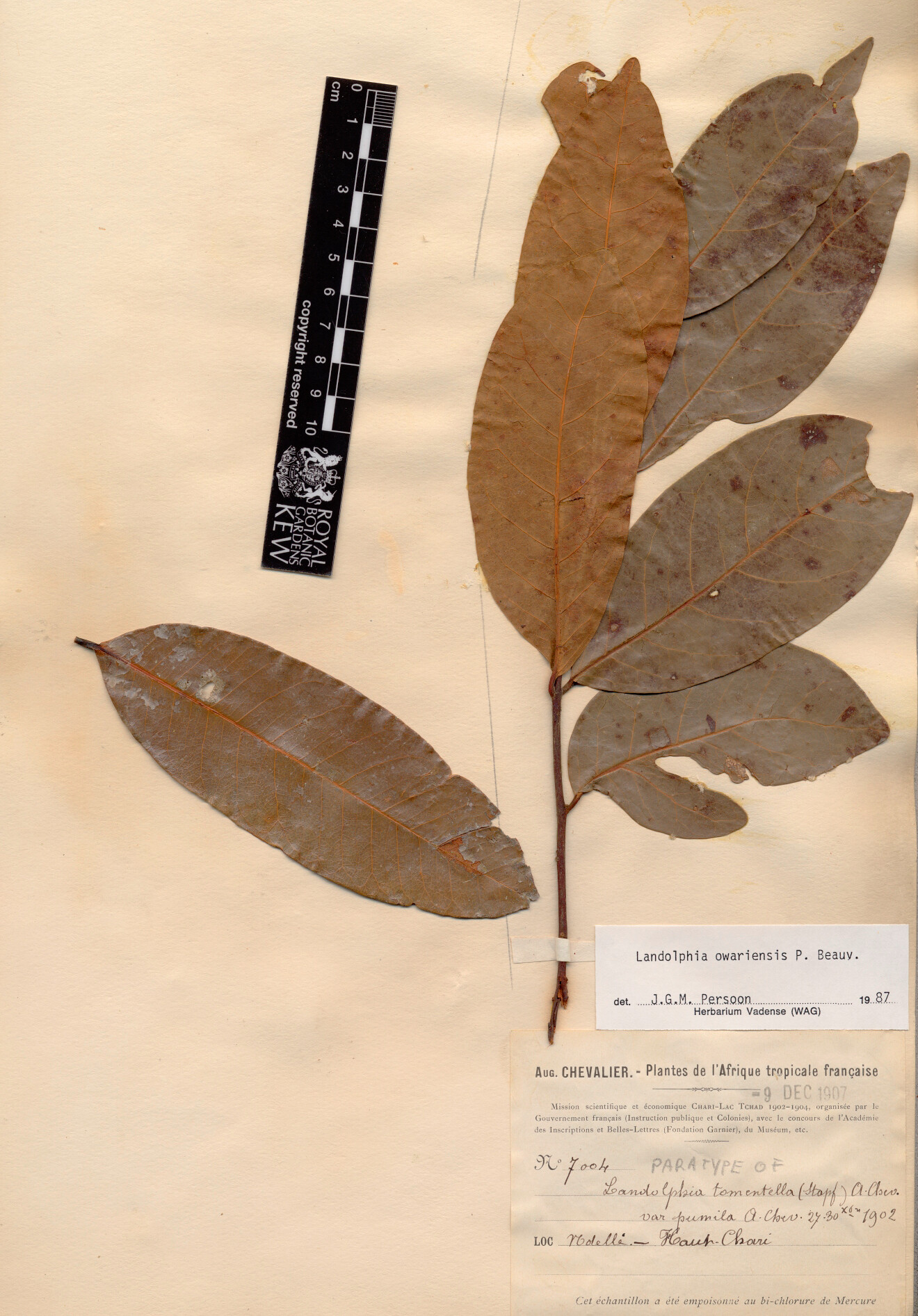
Specimen of wild rubber plant (Landolphia owariensis) collected in the French Congo by botanist Auguste Chevalier in 1902. Now in the Herbarium Catalogue of the Royal Botanic Gardens, Kew.
The Congo river as a transportation infrastructure. Source: Harry Johnston, George Grenfell and the Congo, vol. I (London, 1908), 495.
Rubber and Rainforest
João D. Sousa, a multidisciplinary researcher at the University of Leuven, has authored three papers on the beginning of HIV-1 cross-referencing phylogenetic research with historical and archival sources on the colonial period to understand why the virus emerged precisely at that time. Sousa’s articles imply that the emergence of HIV was not simply coincident with European colonialism in the Congo basin, but a consequence of its effects on physical space and social structures.17
Equatorial Africa, home to the second largest rainforest in the world, was unknown to Europeans until Henry Morton Stanley charted the entire length of the Congo River in 1877. King Leopold II of Belgium took advantage of Stanley’s surveys to lay claim to an enormous area, roughly coinciding with the river basin, and called it Congo Free State. In 1885, the Berlin Conference granted international legitimacy to the new colony, which didn’t belong to Belgium but was a personal domain of King Leopold. While the Conference did not establish the boundaries of African colonies—a process completed only in the following years—it inscribed two key principles of colonization: effective occupation, the requirement for European nations to hold a territorial presence in order to claim political sovereignty, and free trade, the possibility for European companies to conduct business anywhere in Africa.18
The Congo region was (and still is) rich in minerals and raw materials highly prized in Europe. The Congo Free State was structured from its founding so as to maximize the extraction of natural resources, and channel the attendant revenues to the King. Even before 1885, European explorers had been setting up trading posts along the shores of the Congo River, often forcing tribal chiefs to sign away the rights to their territories. In 1891, all the land that was not inhabited or cultivated (according to European definitions), was declared vacant and made property of the Crown, which then distributed it to a number of concessionary companies headquartered in Belgium. The Congo River and its tributaries were the main transportation artery, with regular steamboat services connecting the trading posts to Léopoldville (the colonial name of Kinshasa). From there, goods were carried to the Atlantic coast, initially on foot by enslaved porters, and from 1898 via a new 400km-long portage railway. This first stage of European presence in the Congo might be called territorial urbanization—a system designed solely for the smooth extraction and circulation of commodities.
In the 1890s, after ivory ceased to be the main Congo export, the global demand for rubber boomed due to the invention of the vulcanized tire. As the African rubber plant (Landolphia owariensis) cannot be cultivated but only grows in the wild, Western companies introduced a system of forced labor to ensure a steady flow of latex. Much of the Congo was transformed “into an enormous plantation on which Africans were obliged to harvest rubber in payment of their taxes.”19 Within two decades, millions of Africans died because of the violence, starvation, and diseases that ensued, a legacy for which the Congo Free State is infamous. Villages were vacated and traditional agriculture declined. With the progressive exhaustion of rubber plants, laborers had to spend time farther away from their homes and deeper in the rainforest. And around 1910, when global rubber prices deflated, large patches of rainforest started to be cleared for the plantation of oil palms.20 Furthermore, the distribution of firearms in exchange for rubber quotas greatly increased the hunting of chimpanzees and the consumption of their meat, as other food sources had become scarce.21
All of this was not limited to the Congo Free State. The region north of the Congo River—where HIV is thought to come from—was at that time part of French Equatorial Africa (from 1903) and briefly of German Kamerun (1911–1916). French administrators mirrored the Belgian concessionary regime, leading to comparable violence and environmental devastation.22
Based on this evidence, Sousa concluded that the early colonial economy created a uniquely permissive window for the transmission of SIV from chimpanzees to humans. As the patterns of forest inhabitation were transformed by colonial violence, the contact with chimpanzee meat became more frequent, leading to a higher possibility of infection from simian viruses. It is not that the virus could not have crossed species before, but rather that the social and ecological turmoil after 1885 exponentially increased the chances of such an event (which is in itself rare) occurring.
Yet, as discussed above, even multiple human infections would have no wider consequence if the virus didn’t find an environment suitable to its survival—and it is here that the urban enters the picture. Sousa found records of extensive shipping traffic down the Sangha river (a tributary of the Congo), connecting the forests of Cameroon to the port of Léopoldville. This route was used by French and German companies operating in the region, as they took advantage of Belgian infrastructure by virtue of the free trade agreement sealed in Berlin. It is, very likely, the path followed by HIV-1.
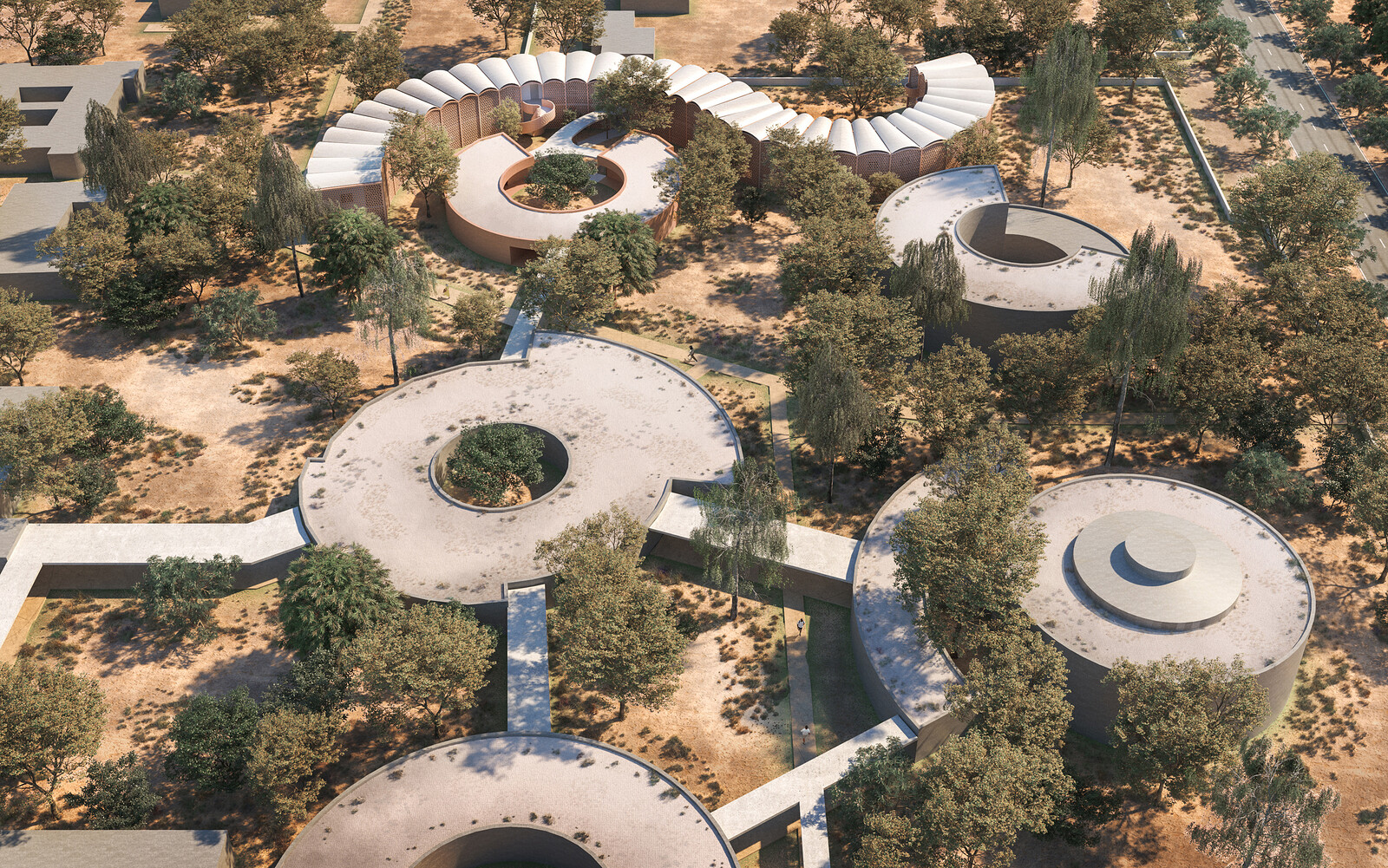
Before colonization, in equatorial Africa there were no cities of a size and form comparable to those in Europe. The site of Léopoldville, on the southern bank of the Congo river, was dotted with villages of a few hundred people each, which in seminomadic fashion could be moved to follow the calendar of shifting agriculture.23 The city was originally founded by Stanley in 1881–83 as twin trading posts, but started to grow only with the opening of the Atlantic railway. Because of its position at the terminus of the Congo river and of the railway, Léopoldville became the main interchange in the colonial trading network. Many of the people who had been displaced by the rubber-related violence migrated there to find work.
One further, crucial consequence of European colonization was the introduction of syphilis to the African interior, where it had not existed before 1885. As is well known, Africa was often feminized and heavily sexualized in the European colonial imaginary; European settlers would largely be men, as women were considered too vulnerable to the “dangerous” tropical climate. As a result, prostitution and concubinage were not simply tolerated by the authorities but an integral part of life in the colonies. African laborers in Kinshasa were also predominantly male; with the severance of social and familial bonds by colonial violence and forced migration, prostitution (hitherto uncommon) became commonplace among African migrants as well.24 Strikingly, Sousa found that the beginning of the HIV epidemic in Kinshasa, estimated between 1919 and 1930 through phylogenetic dating, coincides with a spike in syphilis cases detailed in colonial reports. Because syphilis magnifies the risk of contracting HIV through sexual contact, it was likely the decisive factor in the onward transmission of the virus.
Far from being a mark of primitivism, the sparse precolonial villages were in fact an optimized adaptation of the indigenous peoples to a natural environment as rich in microbes as the African rainforest: limiting settlement size and population density was a highly effective way of avoiding the spread of infections. By contrast, the European colonial city can be conceived as an alien ecology, which amplified the pathogens that had been unleashed in the forests.
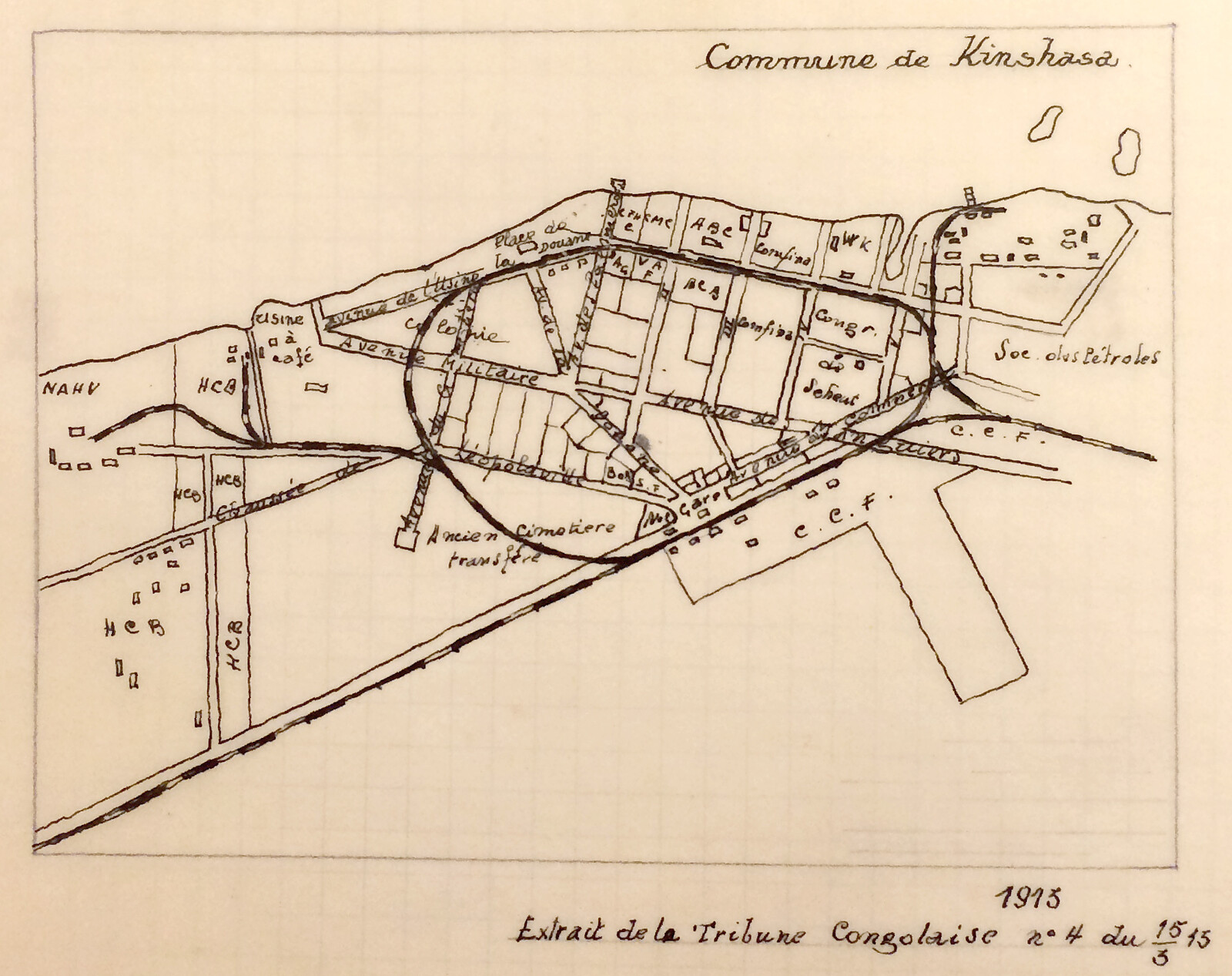
Plan of Kinshasa/Léopoldville in 1915. The acronyms indicate the warehouses of the different concessionary companies. Source: Léon Henrard, “Apercu de l’histoire de Léopoldville,” 1958, 95 Info, Archives Africaines (Brussels).
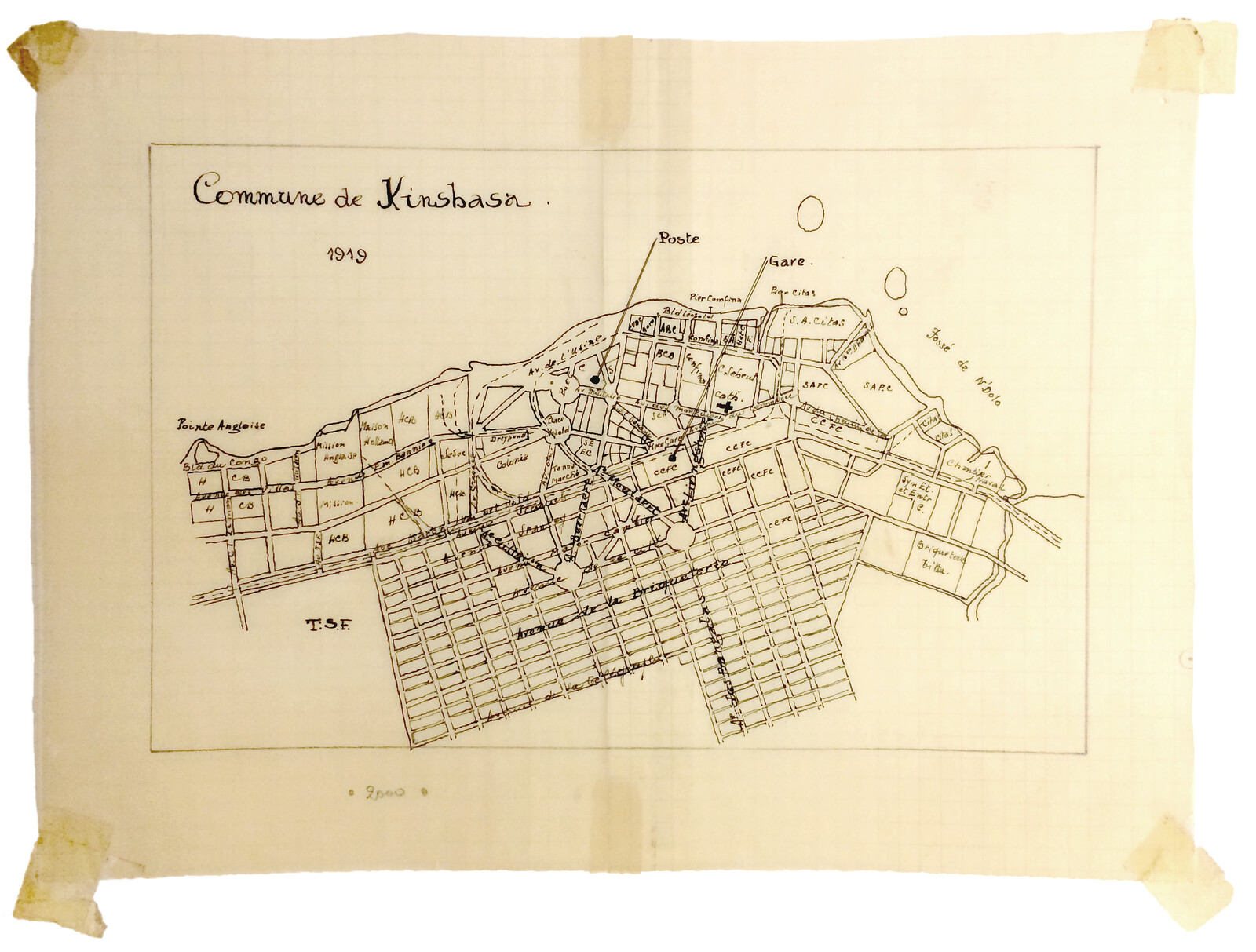
Plan of Kinshasa/Léopoldville in 1919. Source: Léon Henrard, “Apercu de l’histoire de Léopoldville,” 1958, 95 Info, Archives Africaines (Brussels).
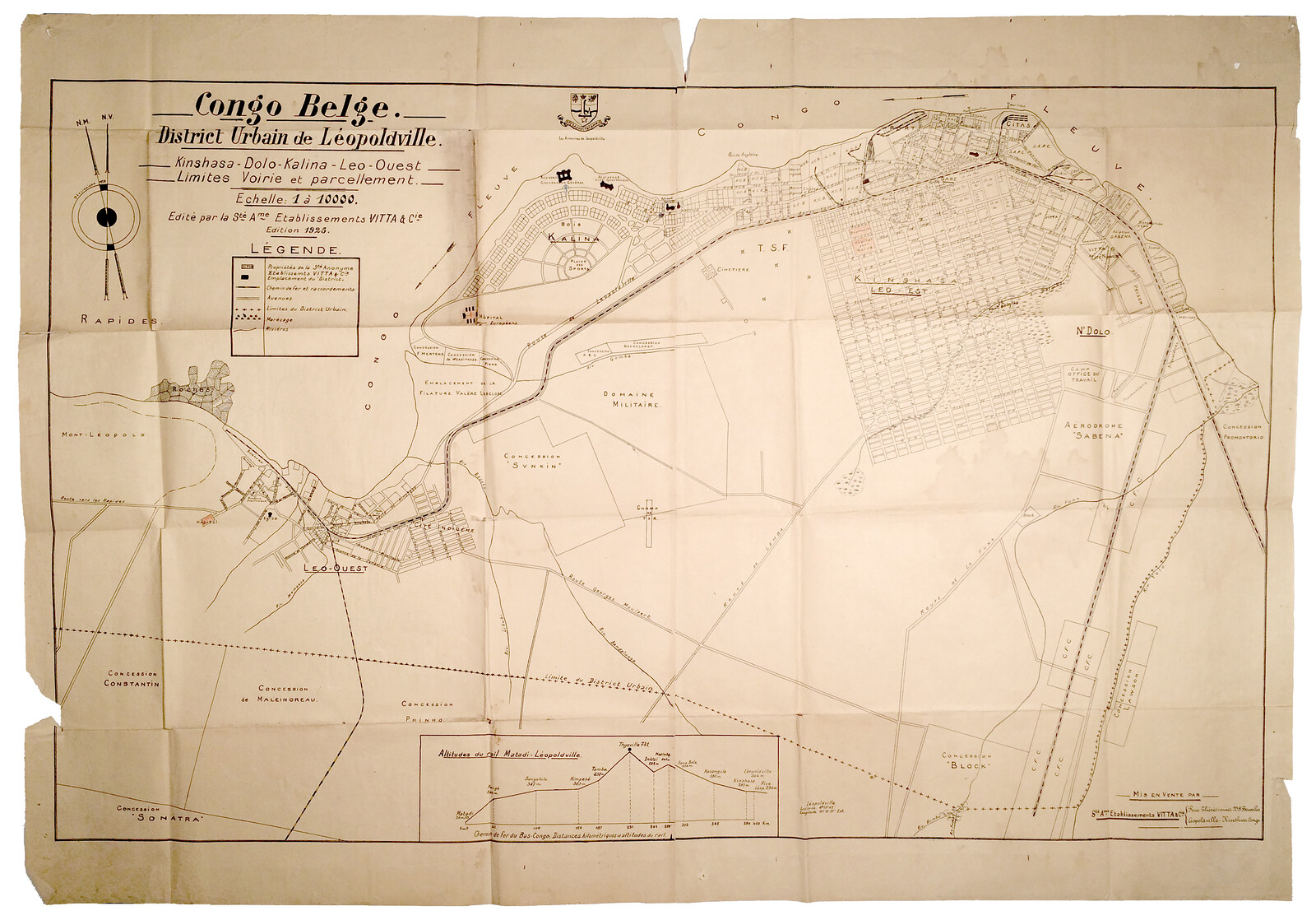
Plan of Kinshasa/Léopoldville in 1925. The gridded expansion to the south is the new cité indigène. Source: Fonds Service Cartographique, 361, Archives Africaines (Brussels).
Plan of Kinshasa/Léopoldville in 1915. The acronyms indicate the warehouses of the different concessionary companies. Source: Léon Henrard, “Apercu de l’histoire de Léopoldville,” 1958, 95 Info, Archives Africaines (Brussels).
Physicians and Planners
As the epidemic was growing undetected in Kinshasa, medicine and sanitation took a larger role in shaping the physical space of the colony. Following the work of Patrick Manson, Louis Pasteur, and others, tropical medicine had become a formal discipline in the 1890s, and was deployed to protect Europeans from the infectious diseases considered native to the tropics. Architecture served the same purpose: in the Belgian Congo as elsewhere in Africa, new typologies of “sanitary houses” were designed to make the local climate (a word that in nineteenth-century usage encompassed microbes as well as the weather) more hospitable to Europeans.25
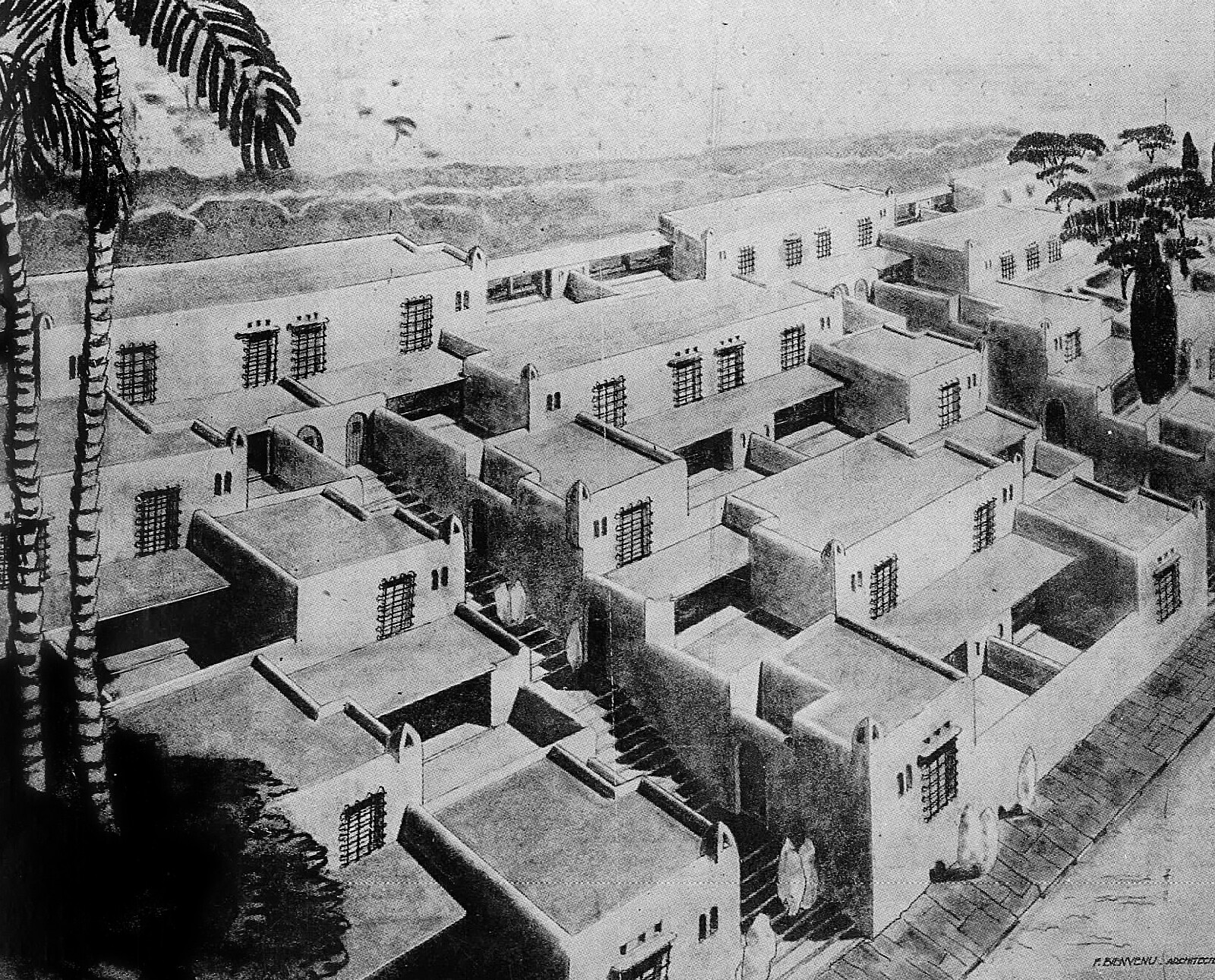
From the beginning, Kinshasa was planned so that European dwellings would be located close to the river, with the workers’ camps farther inland in what came to be called cité indigène. When the number of immigrant workers started to grow, Europeans became more explicitly concerned with the management of the African population. After 1915, what had started out as camps were replaced by a gridded street plan, and from 1923, European companies were required to build new houses for their workers. Despite the fact that native areas were “deliberately kept semi-rural by the colonizer to distinguish them from the more urban and modern European quarters,” the housing was presented as the civilized and benevolent alternative to traditional African dwellings.26
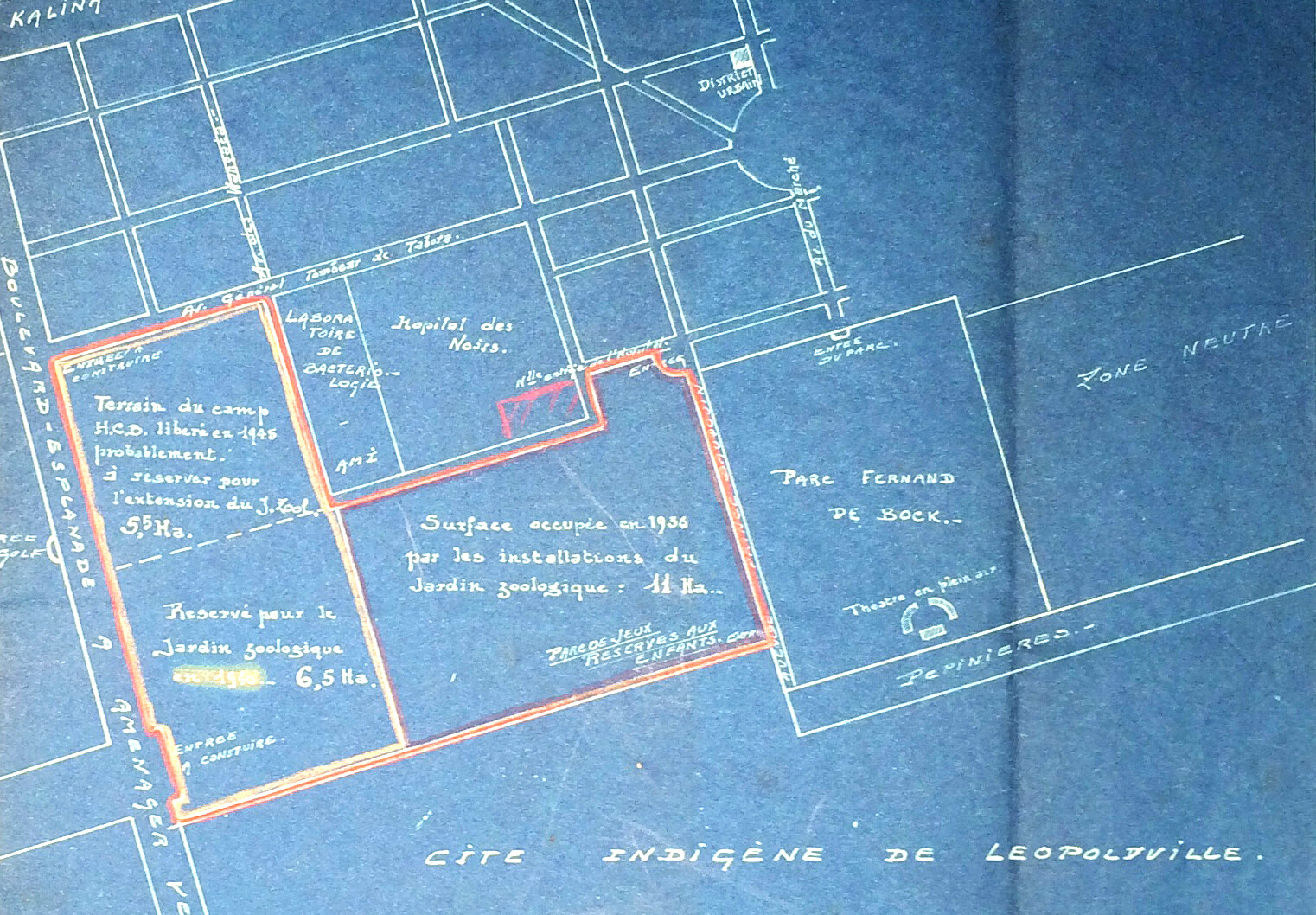
In the 1920s, sanitary discourses entered urban planning in a more radical form, as the principle of spatial segregation took hold. In European cities this was manifested in the zoning legislations that sought to keep apart the different urban functions (housing, industry, leisure) on sanitary grounds. At the same time, in the colonies, the separation of Europeans and non-Europeans was justified with the need to shield the former from diseases (such as malaria) supposedly harbored by the latter.27 Using medical knowledge to grant racial theories a new level of pseudoscientific legitimacy, colonial administrators formalized and enforced residential segregation. In Douala, the larger city of the German Kamerun, the chief physician went even further, arguing that the African part of the city had to be separated from the European one by a “neutral zone”—a strip of vacant land one kilometer wide that would minimize the possibilities of contagion. The concept of the neutral zone was subsequently taken up by colonial planners all around Africa, and by architects too.28
In October 1928 Auguste Tilkens, governor general of the Belgian Congo, wrote to the Ministre des colonies in Brussels, relating his visit to Léopoldville which he had undertaken to study the implementation of a zone neutre. In the letter, he proposed a band of empty land to be carved between the European quarters and the cité indigène. The neutral zone was built soon thereafter, with the additional enforcement of a strict regime of controlled movement and curfews to keep the two populations apart. Yet the neutral zone of Léopoldville—effectively a no man’s land—quickly became a site of sexual encounters between white men and native women.29 Here the history of the city intersects with the virus again, as the very urban device designed to protect the health of Europeans likely played an unwitting role in the ongoing transmission of HIV.
Coda
Colonialism transformed physical space at every scale, from microscopic to urban to planetary. In subjecting the tropical regions of the world to regimes of capitalist production, it reorganized preexisting balances between the natural environment, humans, and other animal species. With the establishment of new networks of free circulation, unwelcome matter like viruses and bacteria began to circulate as well. And with the construction of permanent urban spaces where there were none, such matter found a new habitat—revealing the misguided nature of Western aspirations to bring order and civilization to the rest of the world.
The environmental history of HIV illustrates how power structures play a key role in shaping “natural” entities and processes: Is a virus that mutated because of human action natural or artificial? To use the words of Bruno Latour, there is quite literally no outside. In this sense, the early stages of HIV bear a degree of similarity to the current situation, as most epidemics that have appeared in the last two decades originate at the shifting frontier between urban and rural. For example, the emergence of SARS in 2003 was related to the increased commercial pressure on wild animals in southern China; the Middle Eastern Respiratory Syndrome (first seen in 2012) to the expansion of cities in the Gulf and the associated farming of previously wild dromedary camels; and Ebola (which emerged in 1978 but resulted in a major epidemic in 2014) with forest fragmentation and peri-urban growth in West Africa. These phenomena are by no means limited to the Global South, as evidenced by the Lyme disease that has been spreading in US suburbs since the 1970s.
Architectural disciplines appear thoroughly unprepared to deal with all this, stuck as they are with a rigid opposition between city and environment. Yet, if one begins to think of “the environment” as a category that includes the microscopic, then “the city” assumes a rather different and more complex sense.
William H. McNeill, Plagues and Peoples (New York ; London: Anchor Books, 1998), 80.
Nicholas B. King, “The Scale Politics of Emerging Diseases,” Osiris 19 (2004): 64.
Jonathan A. Patz et al., “Unhealthy Landscapes: Policy Recommendations on Land Use Change and Infectious Disease Emergence,” Environmental Health Perspectives 112, no. 10 (2004): 1092–98; Kate E. Jones et al., “Global Trends in Emerging Infectious Diseases,” Nature 451, no. 7181 (2008): 990–93; Stephen S. Morse et al., “Prediction and Prevention of the next Pandemic Zoonosis,” The Lancet 380, no. 9857 (2012): 1956–65.
World Health Organization, 2017 data, ➝.
Jessica M. C. Pearce-Duvet, “The Origin of Human Pathogens: Evaluating the Role of Agriculture and Domestic Animals in the Evolution of Human Disease,” Biological Reviews 81, no. 03 (2006): 369; Nathan D. Wolfe, Claire Panosian Dunavan, and Jared Diamond, “Origins of Major Human Infectious Diseases,” Nature 447, no. 7142 (2007): 279–83.
Dorothy Porter, Health, Civilization and the State: A History of Public Health from Ancient to Modern Times (London: Routledge, 2006), 40–43.
Michel Foucault, Security, Territory, Population: Lectures at the Collège de France, 1977–1978 (New York: Picador, 2007), 4–23; Porter, Health, Civilization and the State, 142.
Jürgen Osterhammel, The Transformation of the World: A Global History of the Nineteenth Century (Princeton: Princeton University Press, 2014), 176–177.
Beatriz Colomina and Mark Wigley, Are We Human? Notes on an Archaeology of Design (Zürich: Lars Müller Publishers, 2016), 110–116.
See among others Susan Sontag, Illness as Metaphor and AIDS and Its Metaphors (London: Penguin, 2002), 102–122, 146–156.
David Arnold, “The Place of ‘the Tropics’ in Western Medical Ideas since 1750,” Tropical Medicine & International Health 2, no. 4 (1997): 303–13.
Sonia Shah, Pandemic (New York: Farrar, Straus and Giroux, 2016), 19.
There are two strains of the virus, HIV-1 and HIV-2. HIV-1 derives from a chimpanzee virus, and can be further divided into four subgroups: M (which is the one responsible for the global pandemic), N, O, and P. HIV-2 derives from a virus of the sooty mangabey, and is confined to West Africa. The fact that all subgroups have been dated to the same period gives further credit to the hypothesis of colonialism having played a decisive role in the emergence of the human virus. Throughout the text I will refer to HIV-1M.
Michael Worobey et al., “Direct Evidence of Extensive Diversity of HIV-1 in Kinshasa by 1960,” Nature 455, no. 7213 (2008): 661–64.
The location could be established with a high degree of certainty because only in southeastern Cameroon did wild chimpanzees test positive for SIV. See Brandon F. Keele et al., “Chimpanzee Reservoirs of Pandemic and Nonpandemic HIV-1,” Science 313, no. 5786 (2006): 523–26. See also Paul M. Sharp and Beatrice H. Hahn, “The Evolution of HIV-1 and the Origin of AIDS,” Philosophical Transactions of the Royal Society of London B: Biological Sciences 365, no. 1552 (2010): 2487–94.
Nuno R. Faria et al., “The Early Spread and Epidemic Ignition of HIV-1 in Human Populations,” Science 346, no. 6205 (2014): 56–61.
João D. Sousa et al., “High GUD Incidence in the Early 20th Century Created a Particularly Permissive Time Window for the Origin and Initial Spread of Epidemic HIV Strains,” PLoS ONE 5, no. 4 (2010): e9936; João D. Sousa et al., “Enhanced Heterosexual Transmission Hypothesis for the Origin of Pandemic HIV-1,” Viruses 4, no. 12 (2012): 1950–83. João D. Sousa, Viktor Müller, and Anne-Mieke Vandamme. “The Epidemic Emergence of HIV: What Novel Enabling Factors Were Involved?” Future Virology 12, 11 (2017).
David Van Reybrouck, Congo: The Epic History of a People (New York: Ecco, 2015), 53.
Aldwin Roes, “Towards a History of Mass Violence in the Etat Indépendant Du Congo, 1885–1908,” South African Historical Journal 62, no. 4 (2010): 639, 645.
Tamara Giles-Vernick, Cutting the Vines of the Past: Environmental Histories of the Central African Rain Forest (Charlottesville: University Press of Virginia, 2002), 126; Van Reybrouck, Congo, 94.
Sousa et al., “Enhanced Heterosexual Transmission Hypothesis,” 1955.
For an eyewitness account see André Gide, Voyage au Congo, suivi du Retour du Tchad (Paris, Gallimard, 1929); more recently, Catherine Coquery-Vidrovitch, “The Upper-Sangha in the Time of the Concession Companies,” Resource Use in the Tri-National Sangha River Region of Equatorial Africa, Bulletin Series, Yale School of Forestry and Environmental Studies, 102 (1998): 72–84.
Michel Lusamba Kibayu, “La typologie des quartiers dans l’histoire du développement de Léopoldville-Kinshasa en République Démocratique du Congo,” Notes de recherche, Institut d’études du développement (Louvain-la-Neuve: UCL, 2008), 9–17.
Amandine Lauro, Coloniaux, ménagères et prostituées au Congo belge (1885-1930) (Lovervale: Éditions Labor, 2005).
Bernard Toulier, Johan Lagae, and Marc Gemoets, Kinshasa: architecture et paysage urbains (Paris: Somogy, 2010), 16.
Luce Beeckmans, “French Planning in a Former Colony: A Critical Analysis of the French Urban Planning Missions in Post-Independence Kinshasa,” OASE, no. 82 (2010): 57.
Philip D. Curtin, “Medical Knowledge and Urban Planning in Tropical Africa,” The American Historical Review 90, no. 3 (1985): 613.
Zeynep Çelik, “Le Corbusier, Orientalism, Colonialism,” Assemblage, no. 17 (1992): 68–71.
Alexandre Cabral, Histórias Do Zaire (Lisboa: Orion, 1956), 45; Conversation of the author with João Sousa, Leuven, 18 January 2017.
Positions is an independent initiative of e-flux Architecture.
Category
Subject
This essay is part of the long-term project Terra Infecta, which investigates infectious diseases in relation to architecture and urban expansion; it is supported by Het Nieuwe Instituut and the Graham Foundation.
Positions is an initiative of e-flux Architecture.






















(2014).jpg,1600)









,-2003,-srgb.jpg,1600)